Silver has been associated with human medicine and healthcare for over two millennia. The ‘father of modern medicine,’ Hippocrates, wrote about using silver to improve wound care around 400 BC. Silver has featured in a wide range of writings during the intervening years, most of which highlight its capabilities, particularly limiting inflammation and infection. The interest in silver in medicine was probably spurred by long‐held knowledge that silver kept many perishable items fresh for extended periods – for example, and silver coins were often dropped into barrels of water and milk on long journeys to slow their degradation. It was not understood then that silver ions are formed under these conditions, interrupting many microbial processes associated with spoilage. This relatively simple piece of science ultimately drove the medical community’s interest in silver.
One example of this type of research is work undertaken at North Carolina State University under Assistant Professor Rohan Shirwaiker. His team has been developing an electrically‐activated silver‐based antimicrobial implant system. They have engineered the application of low-intensity direct and alternating current mechanisms to a silver‐titanium implant system to release silver ions that kill or neutralize bacteria on and around the implant. A small power circuitry that can be integrated into the implant design creates a potential difference between the implant’s silver and titanium components. The conductive body fluids surrounding the device result in a small electrical current via the release of antimicrobial silver ions. Such a system can be used in implants to prevent or treat device‐associated infection. With the growing number of implant procedures, including total hip and knee joint arthroplasties, such innovations in silver-based antimicrobial technology can significantly improve patient outcomes while reducing medical expenditure. They indicate negligible toxicity. Modern-day medical uses of silver began at the turn of the 19th century when surgeons used silver sutures to help minimize post‐operative inflammation. Later in the 1800s, silver nitrate eyedrops were introduced as an antiseptic (to reduce neonatal conjunctivitis). The following century saw World War I soldiers take silver leaf into battle to help fight infection if they were injured in the trenches. Silver was increasingly used to treat everyday ailments such as sore throats and tonsillitis. This increase in usage was accompanied by the identification of argyria, a rare condition associated with the gradual accumulation of silver compounds in the body and characterized by skin discoloration in the most extreme cases.
Alexander Fleming’s discovery of antibiotics in the late 1920s saw a reduction of interest in silver’s use in medicine for a short period, but this was reignited in the 1960s by the work of Professor Carl Moyer, who was Chairman of the Department of Surgery, Washington University, Missouri. Moyer recognized the potential of silver salts to be used to treat severe burns injuries. In a paper presented at the 69th annual convention of the U.S. National Medical Association in 1964, Moyer described: “A personal experience during 25 years with applying dressings continuously wet with 0.5% silver nitrate to chronically infected open wounds and to thin split‐grafts on surfaces that rejected them repeatedly, had demonstrated that silver nitrate in this concentration cleared the ulcers of organisms such as pseudomonas, staphylococci, streptococci, and proteus quickly and that tiny stamp‐type skin grafts would take and increase rapidly when covered continuously with 0.5% silver nitrate.
Moyer published his experiences with silver nitrate widely, which spurred further research and subsequent improvements to silver-based treatments for burns. Soon after Moyer published his silver nitrate work, a surgeon based in New York, Charles Fox, developed silver sulfadiazine (SSD), which is a topical antibiotic formulated to contain an atom of silver in place of a hydrogen atom found in the standard antibiotic molecule (see figure 1).
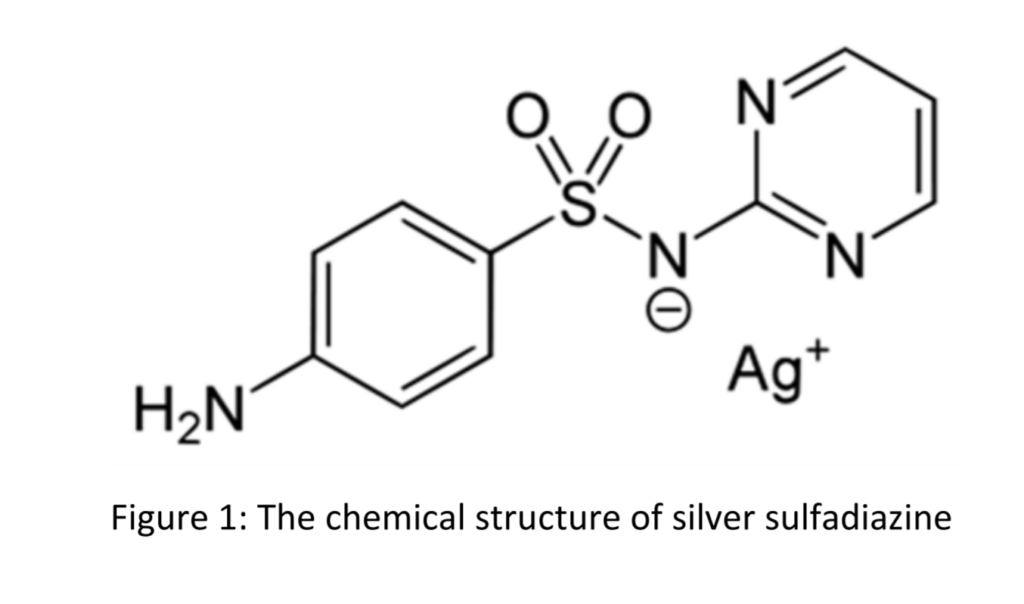
Fox spent years researching SSD and was particularly interested in its mechanism of action; that is, the specific route by which silver and the sulfadiazine combined to offer an effective and safe way to treat severe burns. In the mid‐1970s, he published a paper which stated: “The efficacy of silver sulfadiazine is thought to result from its slow and steady reactions with serum and other sodium chloride‐containing body fluids, which permits the slow and sustained delivery of silver ions into the wound environs.
Until very recently, SSD remained one of the most widely‐used substances of its type in treating burns. A 2016 review concluded that some newly developed non‐silver burn dressings could result in faster healing than SSD. Still, it remains a worthy alternative if treatment with more modern dressings is not an option for any reason. This underlines the enduring value of a fifty‐year‐old silver‐based medical technology in the contemporary world. More modern treatments may have partially usurped SSD, but the research of Fox, Moyer, and their peers has undoubtedly paved the way for other silver technologies to reach the market. Today, dozens of different silver‐containing dressings are commonly available from specialist wound care companies worldwide, such as Smith & Nephew, J&J, Hartmann, and B. Braun. Beyond wound care, silver is used in a range of applications to minimize or prevent infection. In 2007 the U.S. Food & Drug Administration (FDA) cleared a silver‐coated breathing tube for sale. The tube, manufactured by C. R. Bard, helps reduce the risk of Ventilator‐Associated Pneumonia (VAP). Given that 15% of patients on ventilators develop VAP on a yearly basis, and over 25,000 of them die because of this infection, this was a significant development. Catheters are often also silver‐coated to help limit a variety of infections.
But what of the future? Silver continues to be the subject of intense R&D efforts, particularly for limiting and preventing infection. As mentioned above, infections associated with implantable medical devices adversely affect patient health, quality of life, and overall healthcare costs. The emergence of antibiotic‐resistant pathogens has made the search for new antibiotics and non‐antibiotic alternatives even more critical. As discussed, silver is one such alternative, and significant efforts are being made to improve the metal’s actual ionization, which is central to its effectiveness as a tool to tackle the infection. Recent research has focused on nanomaterials, chemical and electrical activation‐based strategies to enhance silver ionization.
One example of this type of research is work undertaken at North Carolina State University under Assistant Professor Rohan Shirwaiker. His team has been developing an electrically‐activated silver‐based antimicrobial implant system. They have engineered the application of low intensity direct and alternating current mechanisms to a silver‐titanium implant system to release silver ions that kill or neutralize bacteria on and around the implant. A small power circuitry that can be integrated into the implant design creates a potential difference between the implant’s silver and titanium components. The conductive body fluids surrounding the device result in a small electrical current via the release of antimicrobial silver ions. Such a system can be utilized in implants for prophylaxis or treatment of device‐associated infection. With the growing number of implant procedures, including total hip and knee joint arthroplasties, such innovations in silver-based antimicrobial technology can significantly improve patient outcomes while reducing medical expenditure.
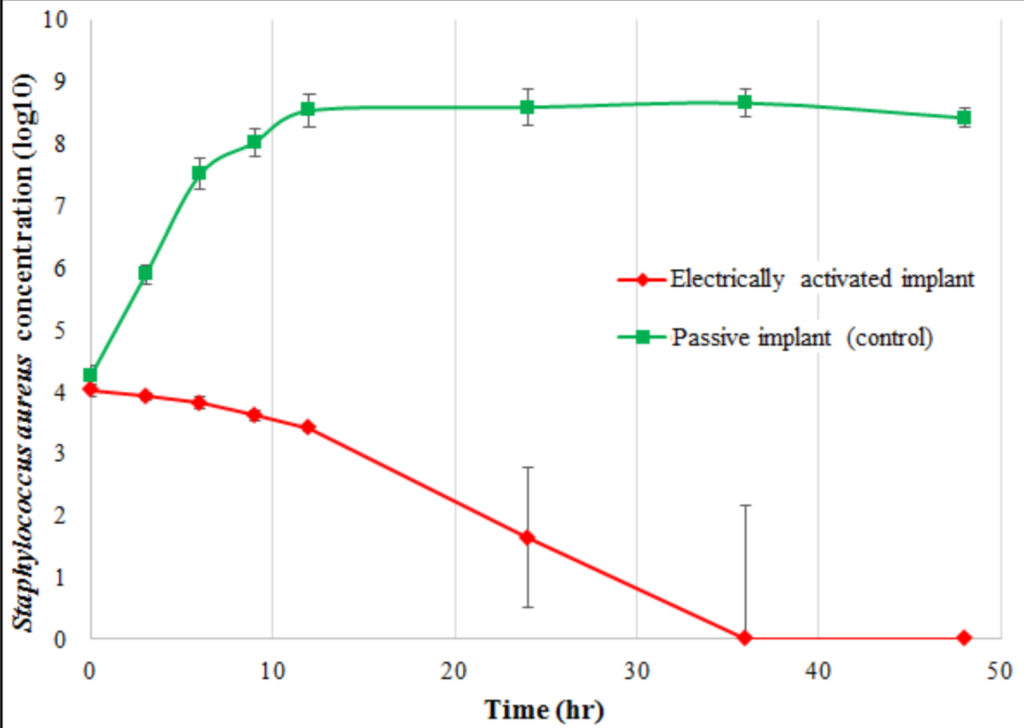
Figure 2: The effectiveness of the electrically‐activated silver‐titanium system in reducing the concentration of pathogenic Staphylococcus aureus bacteria is illustrated over 48 hours in comparison to a passive control device.
Silver has attracted much attention as a potent, broad-spectrum, and natural antimicrobial agent since ancient times because of its nontoxic nature to the human body at low concentrations. It has been used to treat various infections and ulcers, store water, and prevent bacterial growth on the surfaces and within materials. However, there are numerous medical and health benefits of colloidal or nanosilver apart from its microbicidal ability, which the medical community has not fully embraced. These include antiplatelet activity, antioxidant effect, anticancer activity, wound healing, bone regeneration, immunity enhancement, and increase in antibioticefficiency. Additionally, silver also provides protection against alcohol toxicity, upper respiratory tract infections, and stomach ailments. Although nanosilver has been proposed for various topical applications, its usage by ingestion and inhalation remains controversial due to the lack of detailed and precise toxicity information. These beneficial properties of silver can be utilized by using silver at very low concentrations, which are not harmful to the human body and environment.